Diabetes
Recommended for Diabetes
View allDiabetes and The Feet
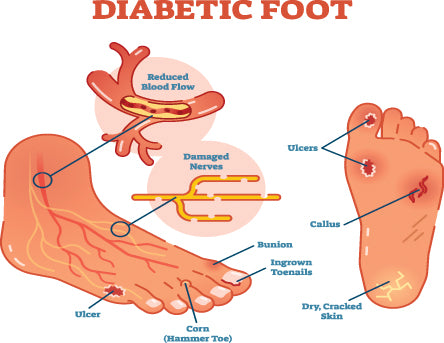
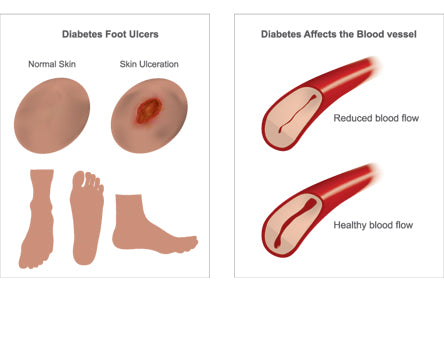
When you have diabetes, you are more susceptible to foot problems developing. Even ordinary problems can get worse and lead to serious complications. These include neuropathy, peripheral vascular disease, calluses, foot ulcers, and poor circulation. If these conditions are not properly treated, they can lead to serious complications and at times they can lead to amputation. If you have diabetes you should talk to your doctor about foot problems that may develop as a result.
What Conditions Can Develop in a Diabetic Foot?
Diabetics can experience multiple different conditions in the feet and other areas of the body. The diabetic foot is one that deserves care and immediate attention at any sign of additional developing pathologies. Some of the conditions that can develop include:
Diabetic neuropathy: If diabetes is not monitored and controlled it can damage the nerves. Damaged nerves on your legs or feet can cause neuropathy, a condition in which you may not feel heat, cold, or pain. You could have a tack or stone in your shoe and walk on it all day and not realize it. If you do not sense pain, you may not feel a cut or sore and it may become infected as a result. It is also possible that the muscles of the foot may not work properly because the nerves that cause them to function are damaged. This can also cause problems.
Peripheral vascular disease: A circulation disorder that affects blood vessels away from the heart. It is poor blood flow in the arms and legs, which can be caused by diabetes. Without a good flow of blood, it takes longer for a sore or cut to heal. This puts you at risk of developing foot ulcers or gangrene (the death of tissue due to a lack of blood.)
Calluses: Calluses are a hard, thickened areas of skin that form as the result of rubbing or pressure on the skin. They tend to occur more often and build up faster on the feet of people with diabetes. Never try to cut them yourself, as this can lead to ulcers and infection. Therapeutic shoes or insoles can be helpful to shift the weight of your foot in your shoe, therefore discouraging calluses from forming.
Foot Ulcers: Ulcers are open sores or wounds on the foot. Foot ulcers are a common complication of poorly controlled diabetes and are most frequently found underneath the big toe or beneath the ball of the foot. If they occur on the side of the foot it is usually do to a poorly fitting shoe. It is important that you do not neglect ulcers, even if they do not hurt. Diabetic foot ulcers can lead to infection in the skin or even the bone, and if not properly treated could end in amputation of a limb. If you have a foot ulcer, avoid walking on it and seek medical treatment right away.
Poor Circulation: Diabetes can contribute to poor circulation, which can make your foot less able to fight infection and heal. Exercise can be beneficial because it stimulates the blood flow in your legs and feet. Your health care provider can also give recommendations for improving your circulation.
Charcot Foot: This condition contributes to a rocker-bottom appearance of the foot due to repeated injury that cannot be felt because of diabetic neuropathy. You can read more about Charcot foot here.
The diabetic foot is one that deserves care and immediate attention at any sign of additional developing pathologies.
What Causes Conditions in a Diabetic Foot?
Foot conditions and pathologies that are the result of diabetes often develop or become worse when the diabetes is not carefully monitored and controlled.
Shoes that do not fit correctly – too small, too tight, or even to large -- can contribute to foot ulcers and calluses and other conditions. Improperly fitting shoes will tend to rub certain areas of the foot or pinch the feet too tight, leading to sores developing in these areas.
Foot conditions and pathologies can worsen if you are not carefully monitoring your diabetes.
What Can I Do to Care my Feet if I have Diabetes?
Monitor Your Diabetes
If you have diabetes it is extremely important to be diligent in keeping it under control. Studies show that keeping blood glucose, blood pressure, and low-density lipoprotein cholesterol levels close to normal can help to prevent or delay foot related problems. See a doctor regularly and follow their recommendations. You may also want to see a podiatrist regularly to pay special attention to your foot care needs. Once a problem develops in your foot it can worsen rapidly, just in the matter of days. Be quick to address any issues that come up and do everything you can for preventative care.
Professional Foot Care
Professional foot care including callus removal and toe-nail clipping is a must for diabetics, especially those with severe diabetes. Taking care of the feet properly can prevent serious problems from ever occurring. Talk to your doctor about recommendations they may have for foot care and what is needed for your type of diabetes.
Wear Adequate Footwear
Proper footwear is also very important part of caring for the diabetic foot. You will want a shoe that fits snuggly (is not a loose and sloppy fit) but also has plenty of room for the forefoot and toes. Choose a shoe that has enough depth and make sure you have 1/3 of an inch of room beyond the end of your toes. It may be helpful to go to a quality shoe store where you can have your foot measured and receive recommendations from professional shoe fitters who are familiar with the diabetic foot.
Custom Inserts and Insoles
Your doctor may prescribe diabetic, heat-molded custom inserts for your shoes, and you will want to make sure to wear them. If you do not have a prescription there are other inserts that work well for diabetics. You will want to choose an insole with a Plastazote top-cover because this material fights against rubbing and friction between your foot and the shoe, therefore protecting the foot. Make sure you shoe does not become too tight when you put the diabetic insole in. If your shoes have a removable liner make sure to remove the liner before putting the orthotic in the shoe.