Plantar Fasciitis (Heel Pain): Causes, Symptoms, and Treatment
Recommended for Plantar Fasciitis (Heel Pain): Causes, Symptoms, and Treatment
View allFeeling a sharp, stabbing pain in the bottom of your foot near your heel? It could be plantar fasciitis.
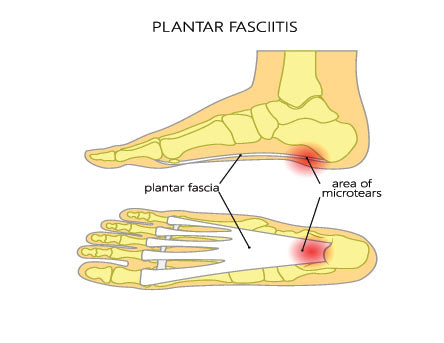
Plantar Fasciitis is the most common cause of heel pain. Your plantar fascia is a thick band of tissue that supports the arch of your foot and connects your heel bone to your toes. If you strain this tissue, it can become swollen and inflamed, thus causing pain in your heel and throughout your entire arch when you stand or walk.
Read on to learn more about the causes of plantar fasciitis, the symptoms of it, and how it can be treated.

Plantar Fasciitis is the most common cause of heel pain. If you treat the symptoms of plantar fasciitis in their early stages then the condition is much easier to manage.
Browse our full collection of insoles for plantar fasciitis.
What Is Plantar Fasciitis?
The plantar fascia is a thick band of connective tissue that runs from your heel to your metatarsal bones at the base of your toes, supporting the arch of your foot. When this band becomes inflamed, it leads to a condition known as plantar fasciitis.
Plantar fasciitis can be an extremely painful condition. This is because each and every step puts stress on the plantar fascia tissue. As you walk or even stand, the plantar fascia can become inflamed, which contributes to increased discomfort and pain that only worsens over time. The pain associated with plantar fasciitis usually begins in the heel, and as the condition becomes severe, it can spread through the entire arch of the foot.
Plantar Fasciitis should be treated as early as possible in its onset because the longer it persists without proper treatment, the longer it can take to heal.
What Does Plantar Fasciitis Pain Feel Like?
Plantar fasciitis pain is often described as a sharp, stabbing, or burning sensation at the bottom of the heel. Some individuals liken it to the sensation of walking on a small pebble or stepping on a nail.
When is plantar fasciitis pain the worst?
You might feel the pain the most in your first few steps after waking up in the morning or after a long period of rest. As your foot warms up and moves, the intensity of the pain might decrease, but it can return after prolonged periods of standing or walking.
This is because, throughout a night of rest, the plantar fascia contracts and micro-healing occurs. The abrupt stretching of the tissue during those first morning steps causes immediate pain and increased inflammation of the plantar fascia. The pain usually decreases after some movement, but often returns after long periods of standing or when you rise from a long period of sitting.
What triggers plantar fasciitis pain?
There are quite a few factors that can trigger a flare-up in plantar fasciitis pain:
- First Steps in the Morning: Pain is often most pronounced upon waking.
- Extended Periods of Standing: Being on your feet for long durations, especially on hard surfaces.
- Starting Physical Activity: Initiating movement after being at rest can trigger pain.
- Inadequate Footwear: Shoes lacking good arch support or cushioning.
- Intense Physical Activity: Especially high-impact exercises such as running or jumping.
- Climbing Stairs: The motion can strain the plantar fascia.
- Prolonged Walking: Especially without periodic breaks.
- Standing Up After Sitting: Pain can be triggered when getting up after being seated for an extended time.
- Wearing High Heels: They can strain the arch and heel.
As you walk the plantar fascia can become inflamed, which contributes to increased discomfort and pain that only worsens over time.
What Causes Plantar Fasciitis?
There are numerous causes of plantar fasciitis that are worth reviewing. The most common are:
- Strain of the plantar fascia
- Improper shoes or support
Strain of Plantar Fascia
Strain and inflammation of the plantar fascia are the primary causes of the heel and arch pain felt with plantar fasciitis. Those who overpronate and roll their feet inward as they walk are more susceptible to developing the condition, but it can show up in all foot types, including high arches and flat feet.
Improper Shoe Support
Often, plantar fasciitis is caused by wearing shoes that do not have proper support. Soft, cushy shoes that bend easily generally aggravate the condition, as well as flat shoes with no support.
Other contributing factors can include:
- Poor foot Mechanics: Issues like flat feet, high arches, or abnormal gait (like overpronation) can stress the plantar fascia.
- Excessive Weight: Being overweight or obese increases strain on the plantar fascia due to increased pressure on the feet.
- Standing for long periods of time: Jobs that require prolonged standing or walking on hard surfaces can contribute to its onset.
- Repetitive Impact Activities: High-impact sports like running, basketball, or dance can increase the risk.
Tight Achilles Tendons or Calf Muscles: This tightness can limit ankle motion, putting strain on the plantar fascia.

Many cases of this painful condition have been found in those who stand or work on cement surfaces all day long.
What Can I Do to Treat Plantar Fasciitis?
Depending on the severity of your condition, you have a few treatment options for plantar fasciitis:
- Wear insoles/orthotics
- Rest and avoid activity
- Avoid going barefoot
- Seek medical care in severe cases
Let’s walk through each of these in a bit more detail.
Wear Arch Support Inserts, Insoles/Orthotics
Basic home treatment is often effective for plantar fasciitis, the most important factor being supportive shoes. Insoles and orthotics can also be very helpful in relieving the pain of this condition. Some of the best arch supports have a deep heel cup that funnels the fat pad of the heel beneath the heel bone, causing it to act as a natural cushion.
Often, people do not realize the difference that supportive shoes and insoles can make in the healing process and turn to more expensive medical options first. But many who focus on supportive footwear, along with light stretching and ice, experience complete relief from the symptoms over time.
Rest And Avoid Activity
If you are suffering from plantar fasciitis, it is important to rest your feet and avoid activities that make your feet hurt. This will allow time for the plantar fascia to heal. Ice the painful area for 15 to 20 minutes once or twice each day, especially after activity.
Over-the-counter pain medication may be needed to reduce swelling when the condition flares up. Gentle toe, calf, and arch stretches can be helpful, especially first thing in the morning before stepping your foot onto the floor. Lightly massaging the foot with a tennis ball a few times throughout the day can also help provide relief. If you need to exercise, you may want to try low-impact sports, such as swimming or riding a bike, instead of walking or jogging. As the condition improves, you can slowly work back into exercise and sports that have a higher impact.
Avoid Walking Barefoot
Once you develop plantar fasciitis, you will want to avoid walking in your bare feet, especially on hard surfaces such as wood floors or cement. This tends to aggravate the condition.
A supportive slipper or house shoe can be worn in the house and should be placed on the foot first thing in the morning before the foot comes into contact with the floor. The immediate relief will be felt. Supporting the arch of the foot first thing in the morning will allow the micro-healing that took place throughout the night to remain intact.
Once your plantar fasciitis is gone, it is generally best to remain in the habit of never walking around barefoot. Those who have developed plantar fasciitis once in their life are very susceptible to developing it again. It is wise to continue selecting supportive footwear and protecting the foot from conditions in which the plantar fasciitis could redevelop.
See A Physical Therapist
A physical therapist may recommend certain exercises or stretches to strengthen your lower leg muscles and stretch the plantar fascia and Achilles tendon, thus stabilizing your ankle and heel.
Gently stretching your plantar fascia several times a day can help reduce tension and promote healing. Start with a light stretch before getting out of bed, and continue stretching after periods of rest or icing. Consistency is key—daily stretching over a month or two can yield significant improvement. Check out our guide on The Best Stretches for Plantar Fasciitis for tips and techniques.
See A Doctor
If your plantar fasciitis pain is persistent after basic home treatment, you should make sure to see a doctor. There are more extensive procedures that can be helpful in relieving the pain, which can include cortisone shots and other procedures. Surgery is rarely needed for this condition and is usually only considered when all else fails, as it is not a desirable option.
Are Plantar Fasciitis and Heel Spurs Related?
Many people with plantar fasciitis also have heel spurs—small bony growths at the base of the heel. Interestingly, heel spurs rarely cause pain themselves. So instead of focusing on the spur, treat the fascia. Reducing inflammation in the fascia is what ultimately brings relief.
How To Choose Insoles For Plantar Fasciitis
If you decide to shop for insoles to help ease the pain of plantar fasciitis or help treat it, here are a few factors to consider when browsing:
- Arch Support: Ensures the foot's natural arch is supported, reducing strain.
- Deep Heel Cup: Look for insoles that stabilize the foot and offer cushioning directly under the heel.
- Material: We recommend you look for insoles that combine some cushion and firmness for comfort. Be careful that the product is not too soft and squishy as this can actually aggravate the plantar fascia.
- Thickness: Make sure to match the thickness to the available space in your shoes and your comfort preference.
- Shock Absorption: Opt for insoles with gel pads or cushioning in the heel region.
- Durability: Ensure the insoles are made of materials that can withstand regular wear; otherwise, they lose their supportive properties over time and effectiveness as a result.
Check out our collection of insoles for plantar fasciitis. We specifically curated these products with the above properties in mind.